Early on in the pandemic, a blogpost came out entitled “Coronavirus: The Hammer and the Dance“. It talked about how, in a pre-vaccine world, to avoid overwhelming our healthcare system, but to allow as much semblance of normalcy as possible, we would need to have successive implementations and releases of various non-pharmaceutical interventions (read: lockdowns, public mask wearing, quarantines, etc.)
As difficult as it was to deal with the reality of that (no matter how much I thought I was mentally prepared for it), it’s perhaps even more tiring now, that in a COVID vaccine world, that with substantial anti-vaccination movements and vaccine hesitancy, and with a new variant (Omicron), that we have to continue this ‘Hammer and Dance’.
A month and a half ago, when I wrote the above, the healthcare system where I live was being overwhelmed. Yesterday (Saturday January 8th), there were no paramedic units available to answer calls. (Toronto Star) (CTV News)

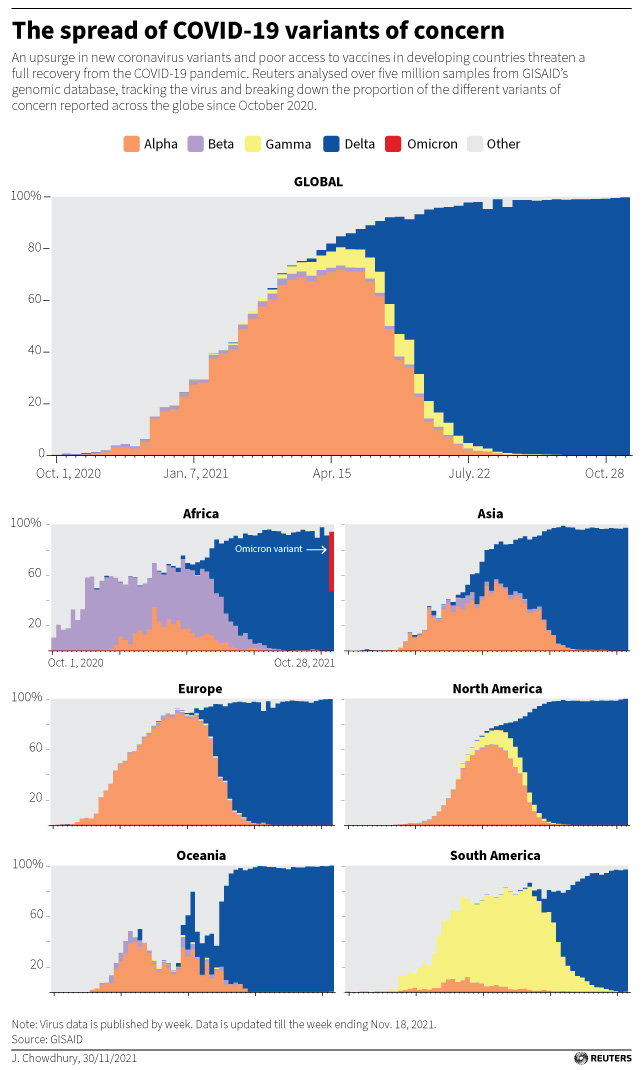
So, that tells you something about the population-wide effects of Omicron, but population effects are equal to individual effects times overall virulence[2]…and what are the individual effects of Omicron, and how is it different from ‘wild-type’, ‘Alpha’, and ‘Delta’?
Thankfully, a wonderful group from the University of Toronto published a paper on the relative likelihoods of hospitalization, ICU admittance, and death for wildtype, Alpha, and Delta.[3][4]
To put it bluntly, Alpha is about 1.5x more deadly than wild-type, and Delta is another about 1.5x more deadly than Alpha.
On top of this, Alpha is also about 30-50% more transmissible than wild-type, and delta is about 50% more transmissible than Alpha.
All three of these variants have much better outcomes if the patients are vaccinated (about 5x better, according to this paper).
So, what does that mean about Omicron?
According to this article, Omicron is 2.7-3.7 more infectious than Delta among vaccinated & boosted individuals, but about the same as Delta among the unvaccinated, suggesting that some sort of ‘immune evasiveness’ is at play.
This article suggests that: “Compared with patients who had the delta variant, omicron patients had a 53% reduced risk of hospitalization, a 74% reduced risk of ICU admission and a 91% reduced risk of death.” (Original paper)
The following chart bears this out:
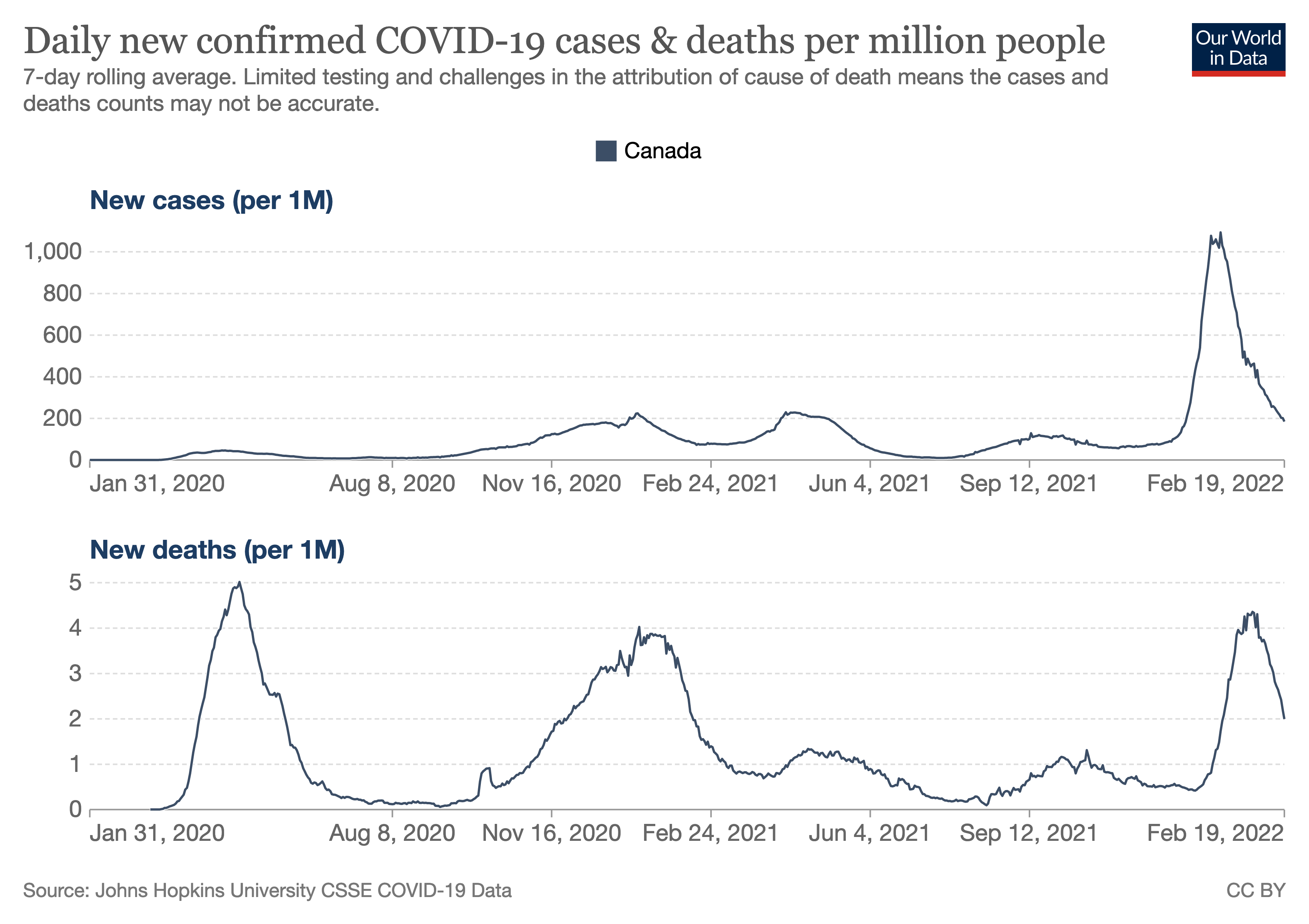
Here, on the lower chart, you can clearly see the five peaks[5] of the (so far) five waves of the pandemic (in Canada). The first peak, in early 2020, of (probably) exclusively wild-type, hitting the entirely unvaccinated population hard, then a (relatively) calm 2020 summer, followed by the second peak in late 2020 and early 2021 likely brought on by winter forcing people indoors, relaxation of restrictions, and complacency. Vaccines began to be approved in December, and were rolled out through the first part of 2021, blunting the third wave (mostly Alpha) and the fourth wave (mostly Delta) in the fall and early winter. As you can see, the fifth wave was quite different, with Omicron blazing through the population, multiple times more contagious than Delta, but also less deadly on a per-case basis, but overall leading to a wave about as large as the initial first early 2020 pre-vaccine wave.
COVID is known to increase the likelihood of pulmonary embolism, strokes, and myocardial infarctions (heart attacks).
So, we’ve all heard about the acute COVID symptoms that are included in the above[6], and there have been some issues with people taking a while to recover from these, but more serious, and less talked-about is the phenomenon of ‘Long COVID’ or ‘Post-COVID syndrome‘.
(It’s relevant to note that we only remember the ‘Long Polio’ part of Polio, simply calling it ‘Polio’. It’s entirely possible that COVID will have a similar long-term impact.)
COVID is known to attack the lungs, the heart, the kidneys, and the brain, among other organs.
As a respiratory disease, it is perhaps not unexpected that COVID would attack and damage the lungs. However, much of the attack on organs done by COVID is thought to be because of extracellular expression of ACE-2[7], the doorway that COVID uses to get into cells and multiply.
As far as neurological symptoms, in addition to the above, there are disturbing indications that COVID’s ‘brain fog‘ has disturbing similarities to alzheimer’s.
So, we know that all kinds of things can happen, but how often do they happen? This study, performed in the highly-COVID-tested population Faroe islands, is likely to have included all of the relevant population that contracted COVID (from April to June 2020, so pre-vaccine, all wild type variant). Four months ‘after’ COVID, half of the population studied continued to have at least one symptom (most often fatigue, lost of smell/taste, and/or joint stiffness).
This much larger study of 270,000 people in the U.S. used six months of HMO data, and found that “over 1 in 3 patients had one or more features of long-COVID recorded between 3 and 6 months after a diagnosis of COVID-19. This was significantly higher than after influenza.” In addition, “[f]or 2 in 5 of the patients who had long-COVID features in the 3- to 6-month period, they had no record of any such feature in the previous 3 months.”
This last feature is especially troubling, considering the large number of reinfections that are occurring, for example. the 650,000 in the UK who likely have been infected twice.
Many who currently have Long COVID are terrified of Omicron, as even mild cases of pre-Omicron variants have had the following effects for some, for more than a year afterwards:
”
“You might have a mild case,” Laurie Bedell, 42, of Pittsburgh, said. “But most people that have long Covid had mild cases.”
She caught the virus in December 2020 and continues to have debilitating pain, fatigue and other symptoms that have transformed her from a healthy, physically active woman to a chronically ill person unable to walk or do any form of exercise for more than 5 to 10 minutes at a time.
…
“I am terrified,” she said. “I don’t know that I would survive another infection.”
”
There is currently only anecdotal evidence, but studies are sure to follow, but:
”
People with long Covid “have good reason to be worried, unfortunately,” said Dr. John Baratta, founder and co-director of the UNC Covid Recovery Clinic in Chapel Hill, North Carolina.
“We have seen people in our clinic who have been reinfected with Covid with the other variants,” he said. “They have new or worsened long Covid symptoms after their reinfection.”
”
So, what do you do?
First and foremost, get vaccinated and boosted (and if you’re eligible, get your second boost). Vaccines remain effective in reducing the effects of acute COVID, even in the age of Omicron.
Vaccines might also reduce the likelihood of long COVID, but research is still inconclusive and ongoing.
Second, get a good mask. A properly fitted N-95 is substantially better than a cloth, surgical, or even KN-95 mask.
Third, continue to limit the amount of time you spend sharing air with people outside your ‘bubble’. COVID is an airborne disease, and transmits much more easily indoors, where ventilation is poorer. Consider contactless delivery, masked curbside pickup, and socially distanced and/or masked walk’n’talks.
The end to this thing may or may not be in sight, but it’s probably not Omicron, and you want to get Omicron as few times as possible.
Stay safe out there.
[1] This is a heart-breaking first-hand account of what hospital front line workers are going through.
[2] Modulo demographics.
[3] There are limitations on the precision of PCR and the classification of variants, but any study that didn’t do whole genome sequencing would have the same limitations. It increases my confidence in the study that they were very precise about what they were measuring.
[4] thanks, Global News!
[5] Eerily similar to the ‘Hammer and the Dance’ article linked above. But it’s very different living through it.
[6] From Johns Hopkins:
”
What are symptoms of COVID-19?
The most common symptoms are:
Cough
Fever or chills
Shortness of breath or difficulty breathing
Muscle or body aches
Sore throat
New loss of taste or smell
Diarrhea
Headache
Fatigue
Nausea or vomiting
Congestion or runny nose
Some of these symptoms are very common and can occur due to many conditions other than COVID-19, the disease caused by the coronavirus called SARS CoV-2. If you have any of the symptoms, contact a doctor or other health care provider, who can assess your risk and help you determine the next steps.
Emergency Warning Signs of Severe COVID-19 — When to Call 911
If you or someone in your household is experiencing any of the following symptoms, call 911 or your local emergency room right away and let the operator know that you are calling for someone who might have COVID-19:
Difficulty breathing
Persistent pain or pressure in the chest
New confusion
Inability to wake up or stay awake
Bluish lips or face
There are other possible symptoms of COVID-19. Call your doctor or health care center regarding any symptoms that are severe or concerning to you.
”
[7] Angiotensin Converting Enzyme 2, a transmembrane protein involved in blood pressure regulation, and extensively studied because of its relation to hypertension.